Originally Published in Quality Health & Wellness Magazine | Fall 2020
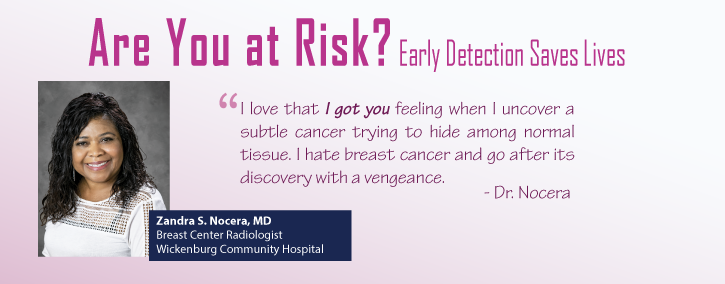
Article Written by: Zandra S. Nocera, MD
Breast Center Radiologist
Wickenburg Community Hospital
Our Approach
I am the breast radiologist at Wickenburg Community Hospital (WCH). Our goal is to provide personalized and compassionate breast imaging to each patient. In the usual setting, a patient with no breast problem will come in for a routine screening mammogram, I interpret the mammogram and forward the results of my findings to the patient’s referring physician. The patient also receives a letter informing her of the result and recommendation. This sequence of events is the standard approach of handling screening mammograms in most breast centers.
Our approach at WCH differs in the handling of what is called a diagnostic mammogram. Diagnostic mammograms are targeted mammograms aimed at solving a problem presented by the patient, such as a palpable lump, nipple discharge, unexplained breast pain, or a problem found on the screening mammogram. Under these circumstances, the mammogram becomes a targeted, problem-solving mammogram, called a diagnostic mammogram. Special mammographic images are taken in the area of concern under my direct supervision to visualize and assess the finding. Frequently an ultrasound of the breast is also performed as an adjunctive study to analyze and characterize the finding.
In our facility, this problem-solving engages my involvement in directing the images obtained and supervising the ultrasound images captured by the ultrasound technician. Once all the mammogram and ultrasound images are completed, my practice is to see the patient personally, do a physical breast examination, re-ultrasound the area as necessary to verify the findings, and correlate the ultrasound findings with the mammographic or physical findings. This personal involvement affords me the chance to explain to the patient why she was recalled for this additional diagnostic imaging and to inquire of other breast concerns.
I have found that so many patients do not understand why they are asked to return and often believe that an error was made on the original mammogram, requiring them to return for corrective images. Often, the additional time and cost can leave a patient feeling agitated and less cooperative. By integrating a personal intervention approach, the patient is afforded an opportunity to be informed of the findings and be provided a recommendation for further action. This recommendation may come in several forms. It may be assuring the patient that everything is normal. I may also inform her that a benign finding was found that requires no additional imaging or that a questionable abnormality was found, which requires sequential imaging to ensure that the finding or lesion is benign. On the other extreme end, I may inform the patient that a biopsy is needed to provide a definitive diagnosis.
In the 33 years I have provided this personalized breast service, it has become apparent that the patient has no idea how we come up with our diagnosis, and many have the opinion that the mammogram provides the complete diagnosis. Nothing could be further from the truth. The diagnosis is arrived at by the careful analysis of the images and further investigation of suspicious findings with ultrasound as needed and, ultimately, a biopsy of questionable abnormality.
For instance, one of the most common concerns I have heard in speaking with patients is their lack of trust in the mammogram because they have had a friend or relative who had a normal mammogram and yet had breast cancer. This misguided opinion provides an opportunity for me to explain, and even illustrate on the mammogram, how breast cancer can be present and yet not seen on the mammogram. First of all, this problem occurs most frequently in women with dense breasts. A dense breast is considered one in which the preponderance of the make-up of the breast is primarily that of glandular tissue and ducts with very little fat. In this case, the breast tissue shows up white or dense on the mammogram because the breast tissue absorbs much of the x-ray beam. The breast’s fatty portion has no density to absorb the beam, so the beam passes through, leaving the area black. Since breast cancers, cysts, and benign solid tumors are derived from the breast’s glands and ducts, they also will absorb the x-ray beam very much like the normal glands and ducts, therefore, showing up white on the mammogram. When the two are superimposed, it is nearly impossible to identify the offending cancer or lump on the mammogram. When the tumor grows in a fatty breast, which is displayed as black on the mammogram, the cancer is a lot easier to spot.
Interacting directly with patients gives me a chance to explain any proposed biopsy procedure and give them clear guidance on what to expect next. This one-on-one contact provides the patient with an opportunity to ask and express other breast concerns. Over the past 33 years that I have been a practicing breast radiologist, this one-on-one approach has been my practice for delivering breast care.
Why I Chose to Practice at WCH
 After completing my residency, I was privileged to work under the apprenticeship of Dr. Avi Ben Ora, formerly of the then Good Samaritan Hospital. He was a key pioneer in the community in the use of film-screen imaging for mammography over the former xeromammography. Dr. Ora was committed to the art of breast imaging, utilizing breast ultrasound and light scan imaging as adjunctive investigative tools. His passion was contagious, and as I ventured into starting my practice in 1987, breast imaging was at the forefront. At Wickenburg Community Hospital, the staff and administrative board shared the same passion for providing quality services. The hospital culture was focused on delivering quality, individualized service, and was not just interested in volume production.
After completing my residency, I was privileged to work under the apprenticeship of Dr. Avi Ben Ora, formerly of the then Good Samaritan Hospital. He was a key pioneer in the community in the use of film-screen imaging for mammography over the former xeromammography. Dr. Ora was committed to the art of breast imaging, utilizing breast ultrasound and light scan imaging as adjunctive investigative tools. His passion was contagious, and as I ventured into starting my practice in 1987, breast imaging was at the forefront. At Wickenburg Community Hospital, the staff and administrative board shared the same passion for providing quality services. The hospital culture was focused on delivering quality, individualized service, and was not just interested in volume production.
The hospital also enjoys the support of the locally formed Pink Ribbon Angels, which not only supports quality care but also provides financial support for those unable to afford breast care. This support is God sent. I was recently analyzing the mammogram of a woman in the Phoenix area whose mammogram showed advanced breast cancer with multifocal bilateral disease and extensive unilateral lymphadenopathy. Upon further investigation, I found out that this was a grandmother who bore the financial burden of taking care of her grandkids and, although aware of the lump for two years, was financially unable to obtain medical treatment. My thought was, “If only there were an organization like the Pink Ribbon Angel Program in her area.”
Impact of 3D Mammography
3D mammography has benefitted the screening program in detecting breast cancer, particularly in patients with dense breasts. In the dense breast, there are multiple layers of superimposed breast tissue, which creates a setting where cancer can hide behind the dense breast tissue. With 3D imaging, many slices are taken throughout the entire breast, allowing the evaluation of each layer of breast tissue unveiling hidden cancers.
Furthermore, in many cases, normal tissue layers are stacked on each other, creating an abnormally dense or white area on the mammogram, giving the illusion that cancer may be present. When this occurs, we, as radiologists, must pursue that dense area and are forced to recall the patient to get additional views. We do focused compression images over the suspected area in an effort to separate the tissue and unveil a potentially hidden cancer.
In many cases, this also invokes an obligatory ultrasound that uses utterly different imaging physics to look at the breast. With this modality, solid and cystic masses interact differently with the ultrasound beam, creating a different image. For example, solid masses absorb the ultrasound beam and show up with a grey image, whereas fluid material does not absorb any of the beams, leaving a hole or black area in the tissue.
On the contrary, because many slices are taken throughout the entire breast, a 3D mammogram often shows no mass but merely a summation of normal glandular tissue, requiring scrutiny of each layer by the radiologist. This method often obviates the need for a callback examination. I feel the 3D mammogram adds to our detection rate and decreases our call back rate for re-evaluation.
Risk Factors & Tools
The most well-understood risk factor for breast cancer is the lifetime exposure to endogenous estrogen and, as with all cancers, any damage to the immune system or DNA.
Most people are familiar with the frequently listed contributors to increasing endogenous estrogen, like weight gain, alcohol intake, inadequate exercise, smoking, sleep deprivation, and its consequent low melatonin levels. Although they may affect your risk factor, these factors are not controllable in preventing breast cancer. For instance, you can prevent lung cancer by not smoking, but there is no such behavioral change that can prevent breast cancer. If you are destined to get breast cancer, you will get it, and there is no known way to avoid it. That’s the bad news. The good news is that if the cancer is detected and removed when it is small, the total cure rate is very high. Therefore, the key to survival is detection, not prevention.
To date, by far, the best tool we have for early detection is mammography! The gold standard is mammography supplemented with targeted ultrasound and sometimes MRI. I ascribe the ACR guidelines, which are annual screening mammograms beginning at age 40 for asymptomatic women. For patients who fall into the high-risk group, screening may begin as early as age 30. In addition, comparison is vital, and the images should optimally be compared with at least three prior exams.
The lifestyle risk factors mentioned above are likewise risk factors for general health, and adopting a change in lifestyle is beneficial for many diseases. My personal favorite is a dietary modification to build the immune system through food choices and supplements. However, in breast health, our focus MUST be on preventing death from breast cancer by focusing on early detection.
Signs & Symptoms to Initiate a Screening
Any change in your breast that concerns you; a lump, nipple discharge, change in the appearance of your nipples such as inversion or red or scaly areolar tissue, change in the skin overlying your breast, such as redness, prominent pores with an orange peel appearance—should trigger a trip to your doctor for evaluation. These are but some of the many possible signs and symptoms of breast cancer, but far and away, the most important concern would be a lump in the breast, particularly a painless lump. This is the reason self-examination is strongly advised. Breasts are often lumpy. If you never do a breast self-examination, examining the breasts for the first time can be a scary venture. When you become familiar with your breast’s topography, you are more likely to detect a lump. Many breasts are so lumpy that even with frequent exams, lump detection is near impossible.
Along this line, many patients have revealed that they don’t examine their breasts because they don’t know how. First of all, there is no magic formula for examining the breast. The whole idea is to get coverage, whether you feel in circles, up and down, zig-zag, or diagonal. As you do this, realize that you may very well not detect any lump. However, it is the best tool we have in between our yearly mammogram. Applying a topical lotion, soap, baby oil, or even putting on a T-shirt facilitates easier detection of lumps.
Surprisingly, many women are more alarmed by breast pain than breast lumps. Note that of all the changes in the breast, breast pain, particularly generalized breast pain, does not rank high on the list as an indicator of breast cancer. Most generalized breast pain is due to hormonal or cyclical changes. Dietary substances such as caffeine and certain supplements and medication may also be a contributor. Less thought about, but relatively common, is a musculoskeletal origin of generalized breast pain, such as costochondritis.
Costochondritis is an inflammation of the cartilage attached to the end of the ribs. Whenever I see a patient presenting with unbearable breast pain, I can almost always predict that costochondritis is the underlying cause. A quick examination and activation of trigger points, generally along the lateral mid rib cage, the cartilage under and inferior to the breast, and along the sternum, replicates the breast pain and usually elicits a loud “ouch” from the patient. This pointed tenderness confirms the musculoskeletal origin and indicates that the pain is not arising from the breast or due to breast cancer. This feedback is often relieving to the patient, and she can leave the office knowing that her problem has been addressed.
The Impact of COVID-19 / Coronavirus
This unprecedented pandemic has challenged the performance of all industries, medicine being no exception. All practices have cut back on staff and some continue to practice through telemedicine. I believe common sense should be utilized in making a health decision. Certainly, if you are in a high-risk area, your thought process will be more prolonged. But as it is in all of medicine, decision making comes from weighing the risks and the benefits.
Being cognizant of patient concerns and the importance of continued patient care, Wickenburg Community Hospital has implemented enhanced infection practices in keeping with CDC guidelines. Temperature checks are made at the door upon entry, housekeeping has increased sanitation measures, and all staff and patients wear masks, which decreases the chance of unwittingly transferring or becoming affected by an asymptomatic carrier.
If you consider that mammography’s purpose is to allow for early detection of breast cancer, a prolonged delay in obtaining the mammogram puts you at risk of discovering breast cancer at a more advanced, less easily treatable stage.