written by:
Karen Smith RN, NMCC, LSSGB
Manager Infection Prevention and Employee Health Chair, Safety Subcommittee at Wickenburg Community Hospital
The Infuenza & RSV Report from ADHS on January 30, 2021 shows that Influenza activity is low in week four of the 2020-2021 season with a cumulative season total 93% lower compared to a typical season.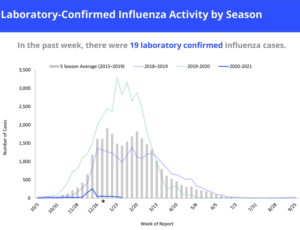
With respiratory diseases often having very similar presentations, one of the things we do here at the hospital and clinics is screen you for Influenza A and B, RSV and Covid-19.
It’s possible that the 2020-1 flu season is not minimal but people with symptoms are avoiding the doctor’s office or hospital ERs to avoid potential Covid-19 exposures. Or perhaps flu season is running late. Flu usually has two waves: in December and January, influenza A predominates then gives way, in February and March, to a surge of milder influenza B cases. We will have to wait and see if a sudden burst of influenza occurs as the winter wears on.
Using the genome sequencing of viral strains, we have learned that some strains spread more readily than others. Indeed, studies have demonstrated that the Covid-19 B-117 variant are up to 50% more contagious than the initial Spring 2020 virus.
The virus is only half of the story in any infection; the other half is the human immune system. A substantial part of the difference in controlling the two viruses may derive from a simple fact: our immune systems have dealt with flu every year for decades, whereas this strain of coronavirus is altogether new to our immune response.
That said, there is some evidence that our immune system is not as COVID-naïve as initially feared. Previous infection with older legacy strains may in fact be beneficial.
Immune memory can be quite amazing — which may be good news for those fearful of viral mutations soon circumventing our current Covid-19 vaccines. During the 2009 H1N1 novel influenza pandemic, researchers noted that older patients had less severe disease. A lead theory was that those old enough to have been vaccinated against swine flu in 1976 likely had a superior immune response, despite the 33-year interval.
Maybe, then, some substantial part of the difference in how well masking-distancing-handwashing seems to protect us lies not with differences in the two viruses but rather an individual’s long-term memory immune repertoire.
Understanding a virus is easy compared to exploration of differences in immunity. The human immune response is composed of many intersecting processes and the whole is much greater than the simple sum of component parts. The all-out scientific assault to fully understand Covid-19 — seems logical and makes for good, scary headlines. Right now, the path to total panic is ever-near each time something new and frightening is found lurking in the viral genome. That’s a standard reaction to all fresh scientific observations until they settle into their proper context. But we should not give over to the temptation to engage in a dizzying “you think that’s bad, well listen to this” competition with each new insight.
To remain even keeled for what’s ahead, we should have a bit more faith in the dexterity of our own immune system. After all, it has gotten us out of our caveman existence, past various plagues, and into the 21st century in one piece. So too should a combination of vaccination and previous infection, along with handwashing, social distancing and mask wearing, continue to carry us forward — however bumpy the ride.




